OH 2020/063
Answer
One service can be billed on day 1, nothing on day 2, and one service on day 3. Additional consultations can also be billed if you attend the patient.
Context
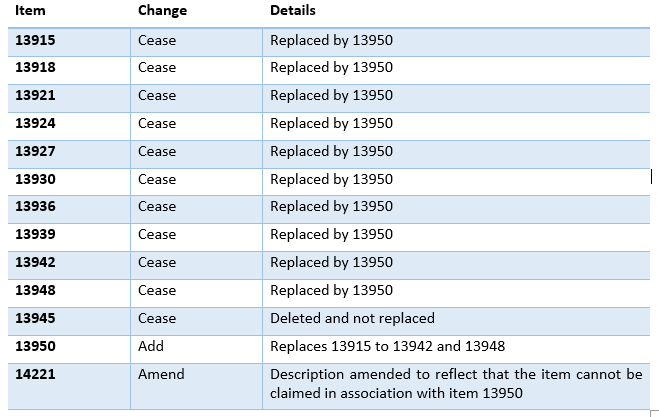
The chemotherapy items in the MBS were updated on 1 November 2020. Accordingly, this information has been updated to reflect the new items and arrangements. Below is a summary of the changes copied from the Department’s website:
This very common scenario is billed by oncologists and haematologists when delivering chemotherapy via an infuser pump such as a folfox.
The typical scenario is that the patient comes in on day 1 to have the pump connected and loaded, is home on day 2 and returns for the disconnect on day 3. Usually the entire course of treatment is billed under supervision arrangements with the medical practitioners not usually attending the patient at all. Oncology nurses typically administer the entire regime.
Here are some examples of reported confusion around the correct billing of this course of treatment using the new item 13950. It was confusing before the item number changes and unfortunately, there are still grey areas.
Doctor A had received advice that Item 13950 can be billed on all 3 days even when the patient was at home on day 2.
Doctor B had received advice that she could bill item 13950 on day 3 when the pump was disconnected, but could not bill item 14221 on that day.
Doctor C was advised he could bill item 13950 everyday while his patients were admitted and receiving a continuous chemotherapy infusion, even if he did not attend the patient (that this could be supervised). This was also not only legally incorrect, but alarming.
Relevant legislative provisions
Health Insurance Regulations 2018
Health Insurance (General Medical Services Table) Regulations (No. 1) 2020
Other relevant materials
1. Academic journal article published in the Journal of Law and Medicine, with discussion on the start and end point of every Medicare service. Medicare Billing Law and Practice: Complex, Incomprehensible and Beginning to Unravel. https://www.ncbi.nlm.nih.gov/pubmed/31682343
2. Pomegranate Health. This Podcast interview includes discussion on where Medicare services begin and end. Billing in Byzantium – https://www.racp.edu.au/pomegranate/view/ep56-billing-in-byzantium
Case law
Stirling v Minister for Finance [2017] FCA 874
PSR Director Case Reports June 2020 – An agreement with an oncologist
“During the review period the practitioner billed more than 19,000 Medicare Benefit Schedule (MBS) services. The Director reviewed this practitioner’s provision of MBS items 112, 116, 13915, 13918, 13921, 13924, 13945 and 14221. The Director had no significant persisting concerns in relation to MBS items 13915, 13921 and 14221. The Director had persisting concerns in relation to the remaining items that:
- the practitioner often billed consultation services in association with chemotherapy and/or line access items. In those circumstances, there was often insufficient documentation of a separate consultation that would justify the billing of MBS items 112 or 116;
- medical records were inadequate. At times, there was no record that the service had been provided by the practitioner;
- MBS item 112 was rendered in circumstances where the patient may not have been eligible for the service; and
- the MBS requirements were not always met. MBS item 13924 appeared to have been billed for subsequent days of treatment where the same infusor was running and MBS item 13945 appeared to have been billed for de-accessing the drug delivery device.
The practitioner acknowledged they engaged in inappropriate practice in connection with providing these items of concern. The practitioner agreed to repay $135,000, to be disqualified from providing MBS item 13924 for 12 months, and will be reprimanded by the Director.“
Departmental interpretation
http://www.mbsonline.gov.au (accessed 24 June 2020)
GN.14.34
Principles of interpretation of the MBS
Each professional service listed in the MBS is a complete medical service. Where a listed service is also a component of a more comprehensive service covered by another item, the benefit for the latter service will cover the former.
MBS online fact sheet title ‘information release #4’ updated 30 October 2020 (note the earlier version was also titled ‘information release #4’ but was dated 20 October 2020. It contained legally incorrect information, which has been retracted. So please do not refer to it if you downloaded it.)
“In order for a service to be claimed under item 13950 there must be an attendance on the patient by the specialist or consultant physician or the health professional providing the service on their behalf. Item 13950 cannot be claimed where the patient is receiving the infusion at home via a pre-loaded pump or ambulatory delivery device and there has not been an attendance on the patient.”
AND
“From 1 November 2020, item 14221 is being amended to clarify that it cannot be claimed in association with the administration of antineoplastic agents for which item 13950 is being claimed, as the MBS fee for item 13950 contains a component to cover accessing of a long-term implanted device for delivery of therapeutic agents. If, at the attendance to disconnect a pump or device, the practitioner further administers antineoplastic agents under a service described by item 13950, then item 13950 may be claimed for that episode of treatment. The administration of antineoplastic agents during the attendance to disconnect the pump or device is considered a separate attendance from the claim associated with the initial loading of the pump or device. Item 14221 cannot be claimed in these circumstances, as item 14221 cannot be claimed in association with a claim for item 13950. Alternatively, if at the attendance to disconnect a pump or device there is no service provided under item 13950, then item 14221 may be claimed for a service associated with the accessing of a long-term implanted device for delivery of therapeutic agents, but only under circumstances where the long-term implanted device is accessed for the purpose of delivery of therapeutic agents (e.g. line maintenance for future access).”
GN.12.31 Services rendered on behalf of medical practitioners
Supervision from outside of Australia is not acceptable
Detailed reasoning
Medicare is a fee-for-service scheme, meaning every service must begin and end somewhere and is distinct from every other service. This basic principle of all fee-for-service schemes is unfortunately sometimes ill-defined in Australia’s Medicare.
Evidence of each service being separate and finite is ubiquitous in the Health Insurance Act by the use of singular terms such as ‘service’ and ‘benefit.’ Section 20A (the bulk billing law) states:
“(1) Where a medicare benefit is payable to an eligible person in respect of a professional service…”
For practical purposes, what is required is that you must select the MBS item that most precisely fits the service you provide and the law requires you to fulfill ALL requirements of each item description, not just some.
It may be helpful to keep in mind that an attendance or consultation is almost always separate from any form of procedure, though there are some exceptions.
So, starting on day 1 of this regimen, it is usual clinical practice that item 13950 will be billed to connect, load and infuse the pump. If you personally attend the patient you can also bill the relevant attendance item such as 116.
On day 2, no service can be billed because no service has been provided while the patient is at home, and the supervision rules provide that you can only supervise a person, not a pump.
On day 3, when the patient comes in for the disconnect and flush, the item number that best fits that service is commonly 14221, on the basis that normal saline is categorised as a therapeutic agent, which is used to flush the CVAD after the disconnect. However, according to the Departmental advice above, if and only if, you administer additional chemotherapy on day 3, then you can claim item 13950 on that day.
IMPORTANT: The overarching statutory requirement of Medicare only reimbursing ‘clinically relevant’ services remains. Therefore, if prior to 1 November 2020 your usual clinical practice did not involve administering a top up dose of chemo on day 3, but from 1 November you change and start doing that, please think carefully about how you would justify this sudden change in your practice as being clinically relevant. Why was it not clinically relevant prior to 1 November but was clinically relevant after. If you find yourself under investigation you will need to be prepared to answer this question.
Items 13950 and 14221 are subject to a restriction, so you can claim one or the other but not both, though whether there is ever an exception is unclear due to poor drafting of the relevant item descriptions.
Best advice is as follows:
a) if the service provided on day 3 is disconnect and flush – then item 14221 would be the appropriate item to bill.
b) if the service provided at the time of the disconnect involved administering a chemotherapeutic agent (separate to that which was being administered by the pump), then 13950 can be claimed, but please note the bolded text above about ‘clinical relevance.’
c) if your patient comes in for a disconnect and flush and you claim item 14221, but later that day there is a valid clinical reason to administer another dose of chemo, it appears you may be able to also claim item 13950, effectively claiming both items on the same date of service (though this is not entirely clear as stated above), but it is suggested you add the time of each service on your claims and submit them together. If you submit them separately they will likely reject. Also keep very comprehensive records about your decision making if you go down this path.
If your patient is admitted for say 7 days, and has a continuous infusion of a chemotherapeutic agent running throughout those 7 days, you CANNOT bill item 13950 each day. The advice Doctor C (above) received was not only legally incorrect, but alarming. To bill in this way would be akin to billing for no service. Again, a decision to write up a push dose of chemo each day in addition to the infusion is not recommended, and would invoke the same question around ‘clinical relevance.’ The overarching requirement of keeping ‘adequate and contemporaneous records’ also applies, and if you haven’t attended the patient once during the 7 days (evidenced by you not having entered anything in the patient’s records), you will not do well if investigated.
It is important to remember that many patients in hospitals have IV infusions running, which contain various drugs that are just as dangerous and toxic as chemotherapy, like ketamine, heparin and morphine. Your colleagues of other specialties do not bill anything other than consultations when they physically come in to see their patients, even though they may be responsible for the infusion for days.
In regards supervision of this particular regimen, the Health Insurance Regulations list item numbers able to be provided by a person other than a medical practitioner (under the supervision of a medical practitioner) and the new chemotherapy item 13950 is not in that list, whereas the previous equivalent items were. Therefore, it is unclear whether the item can be supervised or whether your personal attendance is required, and to compound matters, the drafting of the item includes both of the words/phrases ‘on behalf of’ and ‘attendance’.
It appears likely that the use of the phrase ‘on behalf of’ was intended to convey supervision but I am afraid this is now a grey area caused by poor legal drafting and what appears to be incomplete incorporation of the new service into the regulatory scheme. Therefore, the best and safest approach (to avoid being the next PSR statistic) is to personally attend when providing this service, or at the very least be close by and ensure you make an entry in the patient’s records about your involvement in the procedure as proximate as possible to the time when the service was provided. Nursing staff can also record details of contact they had with you during the treatment being delivered.
PLEASE NOTE – the regulations clearly state you can only supervise a person, you cannot supervise a pump. This is why you cannot bill on day 2. You also cannot supervise a patient or a family member. The people you can supervise are usually nurses and technicians.
Examples and other relevant information
Remember if you are bulk billing you must obtain the patient’s signature on the bulk bill form. See BB 2020/061
If you claim anything on day 2 it would be expected that it would be an attendance item for a home visit.
The supervision arrangements in the Regulations make clear you must have direct involvement in every service you provide, not just the first service in a course of treatment. Evidence of your direct involvement in every Medicare item number you claim should be in the patient’s clinical records.
If there is no ‘adequate and contemporaneous record’ in the patient’s notes and you have been billing item 13950 for 7 days, you would not do well in a PSR investigation. If you are unsure about record keeping requirements you may like to consider doing our online course linked below.
The Private Health Insurers (PHI) are unable to reimburse any service under their legislation without an admission. Given there will be no admission on day 3 (it’s a 5 minute service) the PHI will not reimburse for item 13950. So you will only be able to bill this on an outpatient basis, usually to Medicare.
Claiming (including supervising) while overseas is impermissible. See GA 2020/065
Please read the PSR Director’s report from June 2020 above, in particular the bolded text. The same principal applies in relation to billing of the new item 13950.
Who this applies to
All oncologists and haematologists.
When this applies
Since the new items were introduced on 1 November 2020
